In 2010, the South Dakota Legislature voted to create a prescription drug monitoring program, basically a central database in which doctors and pharmacists can enter the prescriptions they issue and look up patients to check their past prescriptions from other providers. The idea was to prevent prescription drug abuse.
For the last six years, pharmacies and dispensers have been required to submit data about the prescriptions they fill, but use of the database to check patients before issuing prescriptions has been voluntary (see SDCL 34-20E-11). Legislators who participated in the 2016 Interim Substance Abuse Prevention Study want to change that. Senate Bill 2 would require prescribers to “review a patient’s prescription drug record” in the PDMP database before prescribing any Schedule II, II, or IV controlled substance. SB 2 excepts prescriptions for hospice patients, prescriptions lasting three days or less with no refill allowed, drugs administered to the patient by a doctor, and emergency situations.
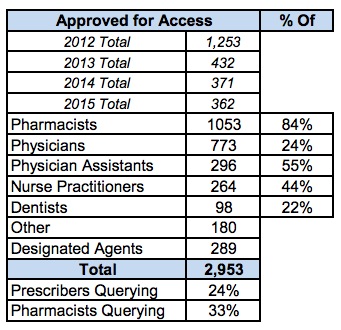
According to South Dakota Board of Pharmacy’s September 2016 statistical report on the prescription drug monitoring program, 84% of pharmacists have applied and been approved for PDMP access, but only 33% of pharmacists were querying the PDMP. Only 24% of prescribers appear to be querying the database. SB 2 intends to bring those numbers to 100%.
The Interim SAPS also recommends Senate Bill 1, which accelerates drug dispensers’ reporting requirements from weekly to daily. The study group offers Senate Bill 3 to spend $318K on a substance abuse education program targeting Native American youth. Finally, the drug abuse study recommends Senate Bill 4 to require the Board of Pharmacy to report to the Senate and House Health and Human Services committees on opioid prescriptions and “any changes or advances” in the PDMP.
Worth noting: it appears that police can request access to these prescription records from the Board of Pharmacy without a warrant. HIPAA says that’s o.k.
A too little, too late over-regulation, especially for professions that pride themselves in their ability to self-regulate. Providers that are not familiar with patients use the monitoring system nearly religiously, so the benefit is there. I see providers regularly take print outs to patients to discuss the prescriptions they have received and to warn of potential abuse and other unsafe situations.
Fortunately, the PDMP has helped providers make informed narcotic prescribing decisions, unfortunately, I fear that many patients that formerly were receiving narcotics from health care providers are being pushed to get pain relief in other, less that legal manners such as heroin.
Self-regulation is a farce. My father, a physician and chief of surgery himself, died of a drug interaction. This bill, as described here, could have saved his life so I believe it deserves serious consideration.